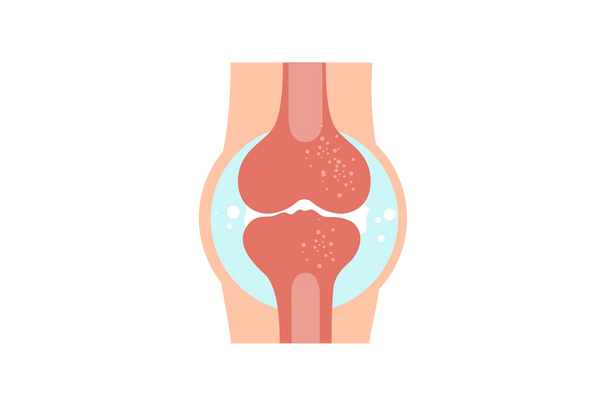
Septic arthritis is a painful infection in a joint that can come from organisms (bacterial, fungal or viral) that travel through your bloodstream. The joints affected are usually the knee, hip, or shoulder.
Septic arthritis quiz
Take a quiz to find out if you have septic arthritis.
What is septic arthritis?
Summary
Septic arthritis is also called infectious arthritis. "Arthritis" simply means inflammation of a joint. In septic arthritis, the inflammation is caused by a bacterial, viral, or fungal infection. The most common is Staphylococcus aureus or staph. These agents reach the joints either from another infection in the body or from a traumatic injury that contaminates the wounded joint.
Symptoms include severe pain in the affected joints, along with redness and swelling. The knees are most often affected but septic arthritis can occur in any joint. This condition is common in infants and the elderly, and medical attention should be received promptly.
Treatment involves draining the infected fluid from the joint, either with a needle (arthrocentesis) or surgery in order to prevent or reduce any joint damage caused by swelling, which can occur very quickly. This procedure is often followed by antibiotics in order to fully eradicate the infection.
Recommended care
You should go to the ER immediately. Treatment entails draining the infected area and providing antibiotics to fight the infection.
Septic arthritis symptoms
Septic arthritis usually affects a single joint, although it can affect multiple joints in about 20 percent of cases. The infection can damage cartilage and bone very quickly, so anyone with these symptoms should see a medical provider as soon as possible. The diagnosis is made through a sample of the joint fluid (aspiration), blood tests, and an X-ray or CT scan of the joint.
Main symptoms
Most people with septic arthritis will experience the following symptoms.
- Sudden-onset joint pain: This pain usually worsens with movement of the joint. Septic arthritis usually affects the knees, hips, ankles, or wrists. However, it may affect the joints in the center of the body, especially among people who use intravenous drugs.
- Swelling: The degree of swelling is usually substantial compared to other causes of joint pain.
- Joint warmth
- Joint redness
Other symptoms
Some people with septic arthritis will experience the following symptoms, but they may differ depending on age or other factors.
- Restricted range of movement in the joint: This may be due to pain or swelling. If septic arthritis affects a joint in the lower extremity, you may be unable to bear weight on that extremity.
- Fever: Most people with septic arthritis will develop a fever. However, older people may not develop a fever because their immune systems are not as strong. In addition, very high fevers or shaking chills are unusual for septic arthritis.
Skin rash
The exact form of rash that may appear in some people is dependent on the organism causing the infection. It is possible to experience:
- Small, fluid-filled skin bumps: Neisseria gonorrhoeae, a common sexually transmitted organism that can cause septic arthritis, may cause this type of rash.
- An expanding, red, ring-shaped rash: Lyme disease may cause this form.
- Ulcers and bumps on the skin: Certain fungal species can cause this form.
Septic arthritis quiz
Take a quiz to find out if you have septic arthritis.
Septic arthritis causes
Septic arthritis is an infection of a joint often caused by bacteria and sometimes fungi. In most cases of septic arthritis, the infection is caused by a single bacteria, but it may be caused by a mix of bacteria if it is caused by direct trauma to the joint. Septic arthritis is often caused by common skin bacteria but can be caused by other bacteria, especially in infants and the elderly. Specific causes include bacteria spreading through the bloodstream, direct trauma or surgery to the joint, having a pre-existing joint disease, having a prosthetic joint, or bacteria spreading from an adjacent joint.
Bacteria spreading through the bloodstream
The most common way that septic arthritis develops is from bacteria that spread through the bloodstream to the joint. There are a number of ways that bacteria can infect the bloodstream, especially in people who:
- Use intravenous drugs
- Have long-standing intravenous catheters
- Have an indwelling urinary catheter
- Have an infection of another organ such as the heart valves
- Have had a dental procedure: Bacteria can also temporarily infect the bloodstream after a dental procedure, and that can provide the opportunity for the bacteria to infect the joint.
Direct trauma or surgery to the joint
Direct trauma or surgery to a joint can cause septic arthritis by directly introducing bacteria to the joint space, which can occur when:
- A wound occurs: This is an especially common cause of introducing outside bacteria.
- Receiving steroid injections: These are administered into a joint for pain.
Having a pre-existing joint disease
Bacteria are more likely to infect a joint that is affected by a pre-existing joint disease. A few types include:
- Rheumatoid arthritis: This is an immune system-mediated inflammation of joints throughout the body.
- Osteoarthritis: This is joint damage caused by normal wear-and-tear of the joint.
- Joint disease of the feet: This commonly occurs in people with diabetes.
- Gout: An excess of uric acid that causes arthritis and inflammation.
Having a prosthetic joint
Having a prosthetic joint following joint replacement surgery increases the risk of developing septic arthritis because prosthetic joints are more easily infected by bacteria. Prosthetic joints are usually implanted after surgical replacement of a damaged joint, such as a knee or hip.
Bacteria that spread from an adjacent bone infection
In some cases, an infection of a bone near the joint (osteomyelitis) can cause septic arthritis if the bacteria spread from the bone to the joint.
Septic arthritis quiz
Take a quiz to find out if you have septic arthritis.
Treatment options and prevention for septic arthritis
Septic arthritis is usually treated with a combination of antibiotic medications and drainage of the infected fluid. Draining the infected fluid promptly is important, as fluid in the joint can continue to cause damage to the joint structures. Antibiotics alone usually cannot completely treat the infection.
Draining the infected joint with a needle
Fluid can be drained using a needle during an arthrocentesis, which is less invasive than surgical options. The synovial fluid is usually clear but may be yellowish or cloudy due to the bacterial infection present. A sample of fluid is examined to determine what type or types of bacteria are causing the infection.
Draining the infected joint surgically
In other cases, the infected fluid may need to be removed in a procedure.
- Arthroscopy: This involves making small incisions near the joint and inserting a camera and surgical instruments through the incisions to clean out the joint.
- Open surgical approach: This involves creating a large incision and directly cleaning out the joint. An open surgery may be more appropriate for septic arthritis of the shoulder or hips, or when a prosthetic joint is involved.
Antibiotic medications
Most people with septic arthritis will be treated with a course of antibiotic medications.
The specific antibiotics used may vary depending on the organisms causing the infection.
- Types: vancomycin, cefazolin (Ancef), nafcillin, ceftriaxone (Rocephin), and/or ceftazidime, among others may be used.
- Form and duration: Antibiotics are usually initially given intravenously and continued for two weeks before switching to a course of oral antibiotics.
Ready to treat your septic arthritis?
We show you only the best treatments for your condition and symptoms—all vetted by our medical team. And when you’re not sure what’s wrong, Buoy can guide you in the right direction.See all treatment optionsWhen to seek further consultation for septic arthritis
If you develop any symptoms of septic arthritis, such as fever, sudden-onset joint pain, redness, warmth, or swelling, you should go to your physician. Your physician can remove some fluid from the joint to test if you have septic arthritis, and then offer the appropriate treatment.
Questions your doctor may ask to determine septic arthritis
- Are you sick enough to consider going to the emergency room right now?
- How severe is your fever?
- Has your fever gotten better or worse?
- Is your fever constant or come-and-go?
- How long has your fever been going on?
Self-diagnose with our free Buoy Assistant if you answer yes on any of these questions.
Was this article helpful?
References
- Septic arthritis. Mayo Clinic. Published December 1, 2018. Mayo Clinic Link
- Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev. 2002;15(4):527-544. NCBI Link
- Horowitz DL, Katzap E, Horowitz S, Barilla-LaBarca ML. Approach to septic arthritis. Am Fam Physician. 2011;84(6):653-660. AAFP Link
- Hassan AS, Rao A, Manadan AM, Block JA. Peripheral bacterial septic arthritis: Review of diagnosis and management. J Clin Rheumatol. 2017;23(8):435-442. NCBI Link
- Zeller JL, Lynm C, Glass RM. Septic arthritis. JAMA. 2007;297(13):1510. JAMA Link