Care Plan
First steps to consider
- Mild pain can be treated at home.
- OTC pain relievers like acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve) can help relieve pain.
- Splints can be used to reduce pain and improve thumb positioning.
When you may need a provider
- OTC medications are not helping the pain or stop helping over time.
- Pain is severe or causes weakness with various movements like pinching and grasping.
Emergency Care
Go to the ER if you have any of the following symptoms:
- Swelling, redness, and increased warmth over the area
- Sudden sharp pain with a visible deformity, especially after a fall or trauma.
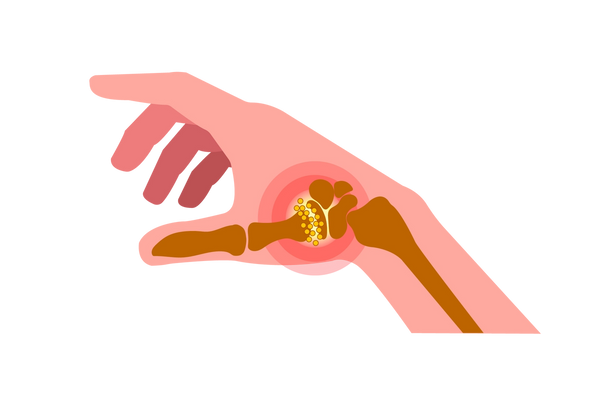
Thumb arthritis refers to inflammation of the thumb joints. There are a number of distinct joints in the thumb, all of which can be affected by thumb arthritis.
What is thumb arthritis?
Summary
Thumb arthritis refers to inflammation of the joints of the thumb. There are a number of distinct joints in the thumb, all of which can be affected by thumb arthritis. The inflammation may be due to "wear-and-tear" or osteoarthritis, a thumb injury, or rheumatoid arthritis.
Symptoms include thumb pain, warmth, redness, and swelling of the thumb joints, limited mobility and possible deformity of the thumb joints, as well as a loss of pinch or grip strength.
Treatments include methods to control pain and alleviate swelling, as well as corrective braces and splints. If conservative methods do not yield relief, a few different surgical approaches may be successful.
Recommended care
You should visit your primary care physician to confirm the diagnosis and discuss treatment options for managing symptoms.
Thumb arthritis symptoms
Symptoms of thumb arthritis are described below, including main symptoms as well as those that are likely over time.
Main symptoms
The main symptoms of thumb arthritis include the following.
- Pain of the thumb: Most people with thumb arthritis will develop pain in the affected joints of the thumb. The pain usually comes on gradually and may be worsened by activities that involve pinching or grasping. The joints may be tender when pushed on.
- Warmth, redness, and swelling of the thumb joints: Some people may develop warmth, redness, and/or swelling of the thumb joints. This is more common in rheumatoid arthritis, which is an inflammatory condition. This is usually less prominent in osteoarthritis since that is primarily due to a physical wear-and-tear of the joint rather than active inflammation.
Other symptoms
Other symptoms that are likely in individuals with thumb arthritis, or that may develop over time, include the following.
- Limited motion of the joints: Some people may develop limitations in their ability to move the joints of their thumb. This tends to happen over time and may be due to the joint associated with joint movement, or due to changes to the structure of the joints from prolonged damage.
- Loss of pinch strength: Some people with thumb arthritis may develop a loss of pinch strength, or a weakened ability to pinch with the thumb and forefinger. They may have difficulty doing things they used to do such as sewing or grasping objects.
- Deformities of the thumb joints: Some people with thumb arthritis may notice deformities in the bones or the joints of the thumb. Some people may notice a hard bump growing outward from the normal bones of the thumb — this may be due to a "bone spur" which can sometimes form in osteoarthritis. Others may notice that the thumb is stuck in abnormally bent positions, which can be seen in rheumatoid arthritis.
What causes thumb arthritis?
The specific joints of the thumb include the carpal-metacarpal (CMC) joint at the base of the thumb near the wrist, the metacarpal-phalangeal (MCP) joint where the thumb leaves the hand, and the interphalangeal (IP) joint near the tip of the thumb. Any of these joints can be affected by a number of different forms of arthritis, each with different causes. Specific causes of thumb arthritis include:
Osteoarthritis ("wear-and-tear")
The most common type of arthritis that affects the thumb is osteoarthritis, which is damage to the joints of the thumb due to normal "wear-and-tear" of the joints over time [3]. The thumb joints are normally covered with cartilage, a substance that acts as a cushion and allows the bones to glide smoothly past each other. Over time, the cartilage covering the ends of the bones degenerates, allowing the bones to rub against each other and cause joint damage. The rubbing may also result in the outgrowth of new bones along the sides of the existing bones, causing deformities and worsening friction. Osteoarthritis usually affects people over 40 years of age and is more common among people who engage in activities that place stress on the joints of the thumb.
Injury to the thumb joints
Injuries to the thumb joints can increase the risk of developing osteoarthritis because joints that have been damaged tend to generate more friction and are more prone to sustaining more damage. Therefore, people who have a history of multiple injuries to the thumb joints may develop osteoarthritis of the thumb at a younger age than they otherwise would have.
Rheumatoid arthritis
Another form of arthritis is known as rheumatoid arthritis (RA), which is an autoimmune disorder that can cause inflammation in multiple joints throughout the body. Rheumatoid arthritis involves inflammation of a fluid within the joints that normally lubricates and cushions the joint. Inflammation of this fluid eventually damages the surrounding cartilage and bone. Rheumatoid arthritis most commonly affects the CMC and MP joints of the thumb.
Treatment options and prevention for thumb arthritis
Thumb arthritis is a chronic condition that usually cannot be completely cured. Therefore, treatments focus on controlling symptoms and slowing the progression of the disease. Specific treatment options include:
Pain medications
People who are experiencing pain from thumb arthritis may benefit from various pain medications. Mild pain can usually be treated with over-the-counter analgesics such as acetaminophen (Tylenol) or NSAIDs such as ibuprofen (Advil, Motrin), or naproxen (Aleve). More severe pain may be managed with prescription pain medications such as celecoxib (Celebrex) or tramadol (Ultram). Some pain medications can be applied directly to the skin, such as capsaicin cream.
Applying heat or cold to the joint
Some people with thumb arthritis may experience a reduction in the pain by applying heat packs to their joint. Others may benefit from applying cold packs or ice to the joint. This can be repeated multiple times per day for relief.
Reducing or modifying movement of the thumb
Some with thumb arthritis may experience a reduction of symptoms by resting their thumb regularly since the use of the thumb can aggravate damage and inflammation. Your physician may recommend wearing a supportive splint to reduce motion of the thumb and allow the joint to heal. Splints may be worn just at night or during the day and night. In addition, some may benefit from using adaptive equipment that is designed for people with limited hand strength to complete everyday activities.
Steroid injections to the joint
If the joint pain is not relieved with reduced activity and pain medications, your physician may recommend trying a course of steroid injections to the joint, although, success rates vary. The steroid can reduce the inflammation in the joint. Steroid injections may be repeated every few months.
Surgery to repair or replace the joint
For those with thumb arthritis that does not respond to other treatments, your physician may recommend surgery to repair or replace the joint. There are a number of surgical options for treating thumb arthritis [8]. After surgery, physical therapy will usually be recommended to aid in the recovery of function.
- Arthrodesis: This involves fusing the bones in the affected joint. This reduces pain and allows the joint to bear weight but limits its movement.
- Trapeziectomy: This involves removing one of the bones in the thumb joint and reconstructing the surrounding ligaments and tendons.
- Joint replacement: A third option is a joint replacement, in which the affected joint is removed and replaced with a prosthetic joint.
Ready to treat your thumb arthritis?
We show you only the best treatments for your condition and symptoms—all vetted by our medical team. And when you’re not sure what’s wrong, Buoy can guide you in the right direction.See all treatment optionsWhen to seek further consultation for thumb arthritis
You should go see your physician if you develop symptoms such as thumb pain, loss of strength, or joint deformities. Your physician can examine your thumb and order imaging tests to determine if you have thumb arthritis, then offer the appropriate treatments.
Questions your doctor may ask to determine thumb arthritis
- Is your wrist pain constant or come-and-go?
- Is your wrist stiffness constant or come-and-go?
- Is your wrist stiffness getting better or worse?
- How long has your wrist pain been going on?
- How long has your wrist stiffness been going on?
Self-diagnose with our free Buoy Assistant if you answer yes on any of these questions.
Was this article helpful?
References
- Arthritis of the thumb. American Academy of Orthopaedic Surgeons: OrthoInfo. Updated December 2013. OrthoInfo Link
- Thumb arthritis. Mayo Clinic. Published June 9, 2018. Mayo Clinic Link
- American Society for Surgery of the Hand. Published 2012. ASSH Link
- Rheumatoid arthritis. American Society for Surgery of the Hand. Published 2017. ASSH Link
- Dias R, Chandrasenan J, Rajaratnam V, Burke FD. Basal thumb arthritis. Postgraduate Medical Journal. 2007;83(975):40-3. NCBI Link
- Morelli J. Use of corticosteroids in osteoarthritis. Arthritis Foundation. Arthritis Foundation Link
- Fowler A, Swindells MG, Burke FD. Intra-articular corticosteroid injections to manage trapeziometacarpal osteoarthritis - a systematic review. HAND (NY). 2015;10(4):583-592. NCBI Link
- Rath L. Surgery for thumb arthritis. Arthritis Foundation. Arthritis Foundation Link